Egg Screening (PGT-A)
To receive PGT-A, you must be able to understand Danish, as the project's information material is in Danish.
As the only fertility clinic in Scandinavia, Aagaard Fertilitetsklinik offers fertility treatment including embryo screening, called Pre-implantation Genetic Testing for Aneuploidies (PGT-A).
Some manage to have their dream of a baby come true after fertility treatment, but for others pregnancy ends in early miscarriage time and again, or they don’t even get pregnant despite treatment.
If fertility treatment fails, you have the following options:
- You can accept that you’ll never have children
- You can adopt
- You can have PGT-A, a screening of the embryo before transfer for implantation
The purpose of using PGT-A is to avoid transferring chromosomally abnormal embryos back into the uterus. Using PGT-A increases the chance of pregnancy, and reduces the risk of early miscarriage.
Who can have treatment?
To receive PGT-A, you must be able to understand Danish, as the project's information material is in Danish.
PGT-A is relevant especially if:
- You are older than 36
- You have had 3-4 early miscarriages after IVF treatment
- You have had 4 IVF treatments without getting pregnant
Don’t hesitate to contact us at the clinic if you need further information about your treatment options.
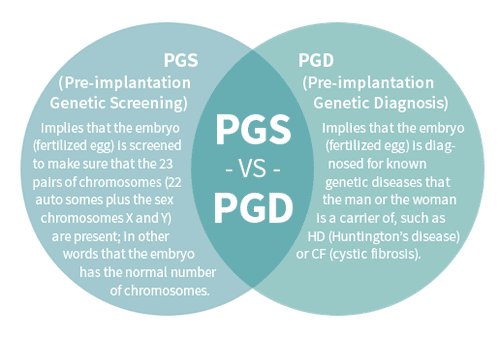
What's the difference between PGT-A & PGT-M?
How PGT-A is performed?
After egg retrieval and fertilization, your eggs will be cultivated in the lab for 5-6 days, to the blastocyst stage. Then each egg (blastocyst) is biopsied by taking out about 5 cells from the part of the egg that will later develop into the placenta. Blastocyst cultivation is necessary to perform the biopsy because it’s not until this stage that it’s possible to tell apart the inner cell mass (which develops into the foetus) and the outer cell mass (which develops into the placenta).
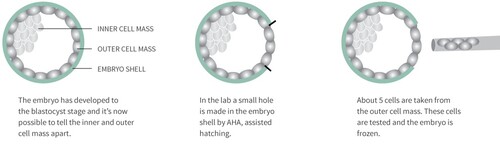
Once the biopsy has been performed, the embryo is frozen and the cells taken from the outer cell mass are tested to establish that the correct chromosome number is present. The testing is carried out with the help of CooperGenomics, England, a lab specializing in genetics diagnosis. They help us identify and reject any chromosomally abnormal embryos. This means we only transfer embryos that have been proved to have 23 chromosome pair; in other words the embryos are chromosomally normal.
Will my embryos be harmed by freezing and thawing?
Blastocysts are very stable when it comes to freezing and hardly ever perish due to freezing and thawing. The chance of pregnancy when transferring thawed blastocysts is almost as high as when using fresh blastocysts (see our results here).
Preconditions for using PGT-A
ICSI
PGT-A can only be used in combination with micro-insemination or ICSI (intracytoplasmic sperm injection). The difference between ordinary IVF treatment and ICSI lies in the way the egg is fertilized. In ordinary IVF, egg and sperm are simply mixed and it’s up to the sperm cells to find their way to the egg. In ICSI a single sperm cell is injected directly into the egg. This is the only way to be sure that the biopsy of the embryo contains genetic material from no other sperm cells than the one that fertilized the egg.
More eggs than in ordinary IVF
In ordinary IVF treatment, 8-9 eggs are retrieved on average. However, when planning for treatment using PGT-A it’s a good idea to retrieve a few extra eggs. There are two reasons for this. Firstly, there is the fact that about 5% of chromosome test results tend to be inconclusive. And secondly, there will probably be a need to reject more eggs, precisely because they are tested for chromosome abnormalities.
Is PGT-A a new method?
The PGT-A method has been known for 10 years. Yet, it is only within the last couple of years that series of treatments have been published.
How safe is the method?
The method is not 100% safe. In some cases the chromosome tests will show, wrongly, that the chromosome number is abnormal although it is in fact normal. This means that embryos may be rejected without due cause.
So far treatment using PGT-A has only been performed in a small number of clinics around the world, and treatment has only just started in Denmark. This means that the number of children born after PGT-A treatment is very small.
Aagaard Fertilitetsklinik has been given permission to perform PGT-A treatment after evaluation and subsequent approval by the Regional Committee on Health Research Ethics.
Our team
The members of the PGT-A and PGT-M team at Aagaard Fertilitetsklinik are our medical director; Aboubakar Cissé, Johnny Hindkjær, laboratory manager and embryologist Helle Ringbøl Bitsch, clinical embryologist Malene Høeg and professor and chief physician, dr.med. Jens Michael Hertz.
